Fact checked – 8 min read
Feeling tired all the time isn’t just a reflection of our ‘normal’ stressful modern lifestyles, sometimes it’s a signal that your body’s iron balance is shifting, so you need to listen to your body and take action early. This case study shows how detecting subtle changes in blood results early on, combined with Nutritional Therapy, prevented iron deficiency and restored wellbeing.
Recognising the early signs
During 2024, this middle-aged male client presented with persistent fatigue and reduced focus. His diet appeared somewhat imbalanced and revealed some clues, which together with his symptoms suggested early iron depletion, when the body’s reserves start to fall before blood counts drop (1). Iron plays a key role in energy metabolism, thyroid conversion, red blood cell production, and oxygen transport (2). Even mild iron insufficiency can lead to tiredness, poor mental clarity, and decreased performance (3).
Without going in to too much detail, this client was also experiencing other red flag symptoms which were causing him to loose blood, partly explaining his iron imbalances and fatigue. In the best interests of patient safeguarding, the client was referred to his GP for further evaluation in order to rule any other malignancies. The cause for the client’s blood loss was initially evident and eventually confirmed by his GP, no other malignancies were detected. The client nevertheless chose to take a more natural route to wellness with my support, and the reasons for the blood loss were eventually rectified naturally with an optimised diet and lifestyle.
Lab findings
Detecting the downwards trend early
Routine testing across 18 months revealed a subtle, progressive but reversible pattern, most notable on the 20/02/25 (Fig.1 shaded pastel), but the downwards trends was already showing during 2024, particularly a mild decline in transferrin saturation % suggesting reduced iron transport capacity (5), and the client was informed of this. Unfortunately due to life circumstances the client was unable to meet until after the July 2025 by which time frank iron depletion was already evident from his blood work.

Haematology: Early signs, but no anaemia yet.
His red blood cell (RBC) indices reinforced this picture of early depletion, a clear downwards shift towards iron deficiency without overt anaemia, again most notable on the 20/02/25, note the significant dip in iron capacity green trend lines (RBC, Hemoglobin, hematocrit) (fig.2).

Key findings on the 20/2/25 (shaded pastel)
Iron (µg/dL)
Major dip highlighted at 20/02/25 to 50 µg/dL a significant drop in available circulating iron compared to 2024 levels suggesting early depletion stage (explains fatigue).
Transferrin Saturation (%)
Dip from 23 to 14.4%. Transport capacity significantly reduced at this point, confirming functional iron shortage.
Ferritin (ng/mL)
Decrease to 39 ng/mL. Low-normal stores consistent with early iron depletion.
Haemoglobin (g/dL)
Stable but mild dip to 13.3 g/dL at 20/02/25 suggests No anaemia but slight variation within normal range (explains fatigue).
Haematocrit (%)
Mild dip to 38.6%, still above lower limit.Slight decline reflecting transient iron shortage, but no anaemia.
MCV (fL)
Dropped from 91 to 87.9 fL, still within normal range, suggests RBC remained normally formed (normocytic); no small RBC formation suspected (microcytosis), nor large RBC (macrocytic) ruling out B12/B9-related anaemia.
RBC (×10⁶/mm³)
Slight reduction from 4.65 to 4.39 to 4.52 suggests RBC stayed within normal limits, no evidence of anaemia but explains fatigue.
Targeted Nutritional Therapy: Restoring balance
A personalised iron-focused Nutritional Therapy plan (5,6,7) was implemented in July 2025, focusing on nutrition education, optimising iron-rich foods (8), food pairing and timing to maximise heme and non-heme iron absorption (9) and other factors that could reduce iron absorption (10). The strategy was intended as a quick fix, but as a restorative, food-first approach that maximised both dietary intake and absorption efficiency. A specially formulated iron supplement, specifically for this client, was recommended to support iron uptake.
A warning on iron supplementation
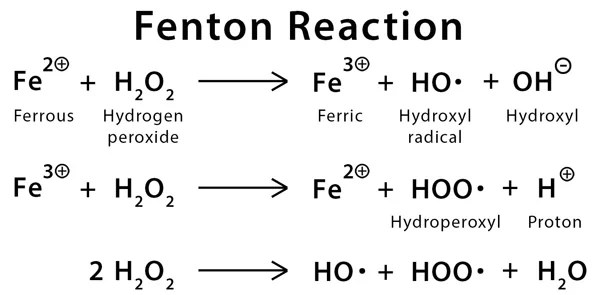
There are many iron supplements on the market, with different chemical forms that determines how well they’re absorbed. The wrong formulation can lead to various gut symptoms and discontinuation. Iron is also highly oxidative in the wrong (inflammatory) environment via the Fenton reaction (Fig.3), which involves the use of free unbound iron ions and hydrogen peroxide to create oxidising radicals liked to premature aging, neurodegeneration and other chronic diseases (4), especially in males who have no natural mechanisms to excrete iron, unlike premenopausal women (menstruation). Therefore, supplementation should be used as a last resort and for the minimum amount of time, particularly during prevention when acute requirements are less critical. Supplementation was ceased after his last blood test on the 9/10/25. Tracking continues.
Recovery and Results
By October 2025, the client reported full resolution of fatigue and a marked improvement in mental clarity and energy. Follow-up testing confirmed the efficacy and success of his intervention:
– Iron increased from 50 → 128 µg/d suggesting improved availability.
– Transferrin saturation improved from 14.4 → 35% suggesting increased iron transport.
– Haemoglobin remained strong at 13.6 g/dL, confirming normal oxygen-carrying capacity.
– Ferritin declined modestly but still within acceptable ranges.
A note about Ferritin
Ferritin is a protein that stores iron inside cells and releases it when the body needs it. It acts like the body’s iron ‘bank account’, and reflects how much iron is in reserve rather than what’s currently circulating in the blood. Although the client’s levels dropped modestly on the 9/10/25, it remained within a healthy reference range (≈30–300 ng/mL). The modest reduction can be explained as it likely reflected increased release of stored iron into circulation (reduced during inflammatory states), as serum iron and transferrin saturation increased significantly following Nutrition Therapy. In other words, Ferritin fell slightly because the body was actively using stored iron to rebuild red cell and functional iron pools, a sign of improved turnover. Over time, it is likely that Ferritin levels will rise as blood and tissue levels stabilises, but this is an area that requires further monitoring and work in progress.
Why early detection and prevention matters
Iron deficiency is the world’s most common nutrient deficiency (11), affecting up to one-third of the population (12). Yet, it rarely develops overnight, it follows a progressive, measurable pattern from depletion, to deficiency, to anaemia. By detecting, taking early action and tracking these subtle trends, Nutritional Therapy can:
– Prevent deterioration into anaemia.
– Reduce the need for medical treatment or more aggressive supplementation.
– Support long-term energy and vitality.
– Detection and tracking of imbalances early on with functional blood testing & analysis
This case exemplifies preventative, prophylactic action in practice, where early testing, careful interpretation of signs and symptoms, blood biomarkers, and personalised nutrition, prevented a potential decline to frank anemia into lasting wellbeing, and an example of how I work with everything health-related, and how prevention and early prophylactic action can easily prevent more serious health complications.
Key takeaways
Detecting small shifts in lab values can hold significant clues. By acting on early warning signs, not waiting for disease to happen, I can help anyone experiencing iron-imbalances / anemia symptoms (or pretty much anything else for that matter) by use of function laboratory testing, personalised nutrition and lifestyle to restore balance naturally, protecting energy, focus, and supporting overall health and wellbeing.
Get touch in touch for a consultation to improve your health especially if you are experiencing any unrelating symptoms.
- Andrews NC. Disorders of iron metabolism. N Engl J Med. 1999;341(26):1986–95.
- Oustamanolakis P, et al. Serum ferritin and iron deficiency in inflammatory and noninflammatory gastrointestinal diseases. Dig Dis Sci. 2011;56(10):2909–16.
- Camaschella C. Iron-deficiency anemia. N Engl J Med. 2015;372(19):1832–43.
- Ganz T, Nemeth E. Iron homeostasis in host defence and inflammation. Nat Rev Immunol. 2015;15(8):500–10.
- Schaefer B, et al. Ferritin, transferrin saturation and iron deficiency in chronic diseases. Clin Chim Acta.2019;495:12–7.
- Alleyne M, Horne MK, Miller JL. Individualized treatment for iron-deficiency anemia in adults. Am J Med.2008;121(11):943–8.
- Short MW, Domagalski JE. Iron deficiency anemia: evaluation and management. Am Fam Physician.2013;87(2):98–104.
- Cook JD. Diagnosis and management of iron-deficiency anaemia. Best Pract Res Clin Haematol. 2005;18(2):319–32.
- Hurrell RF, Egli I. Iron bioavailability and dietary reference values. Am J Clin Nutr. 2010;91(5):1461S–7S.
- Morck TA, Lynch SR, Cook JD. Inhibition of food iron absorption by coffee. Am J Clin Nutr. 1983;37(3):416–20.
- Zimmermann MB, Hurrell RF. Nutritional iron deficiency. Lancet. 2007;370(9586):511–20.
- World Health Organization. Nutritional anaemias: tools for effective prevention and control. Geneva: WHO; 2017.



You must be logged in to post a comment.